The Claims Dossier
Story Two -
Modern Treatment Methods clause
Some time back, one of our Clients' claim for a Knee Replacement Surgery was approved, albeit with about 75% deduction from the claimed amount.
Why?
Because the Insurer applied the Reasonable and Customary clause.
The Insurer was of the opinion that a Knee Replacement Surgery should cost about 75% lesser than what our client was claiming. The Insurer had considered costs in similar hospitals in the geography.
But what the Insurer missed was the fact that we had gotten our client covered under “Modern Treatments” under the policy. Moreover we had gotten this cover with no sub-limits.
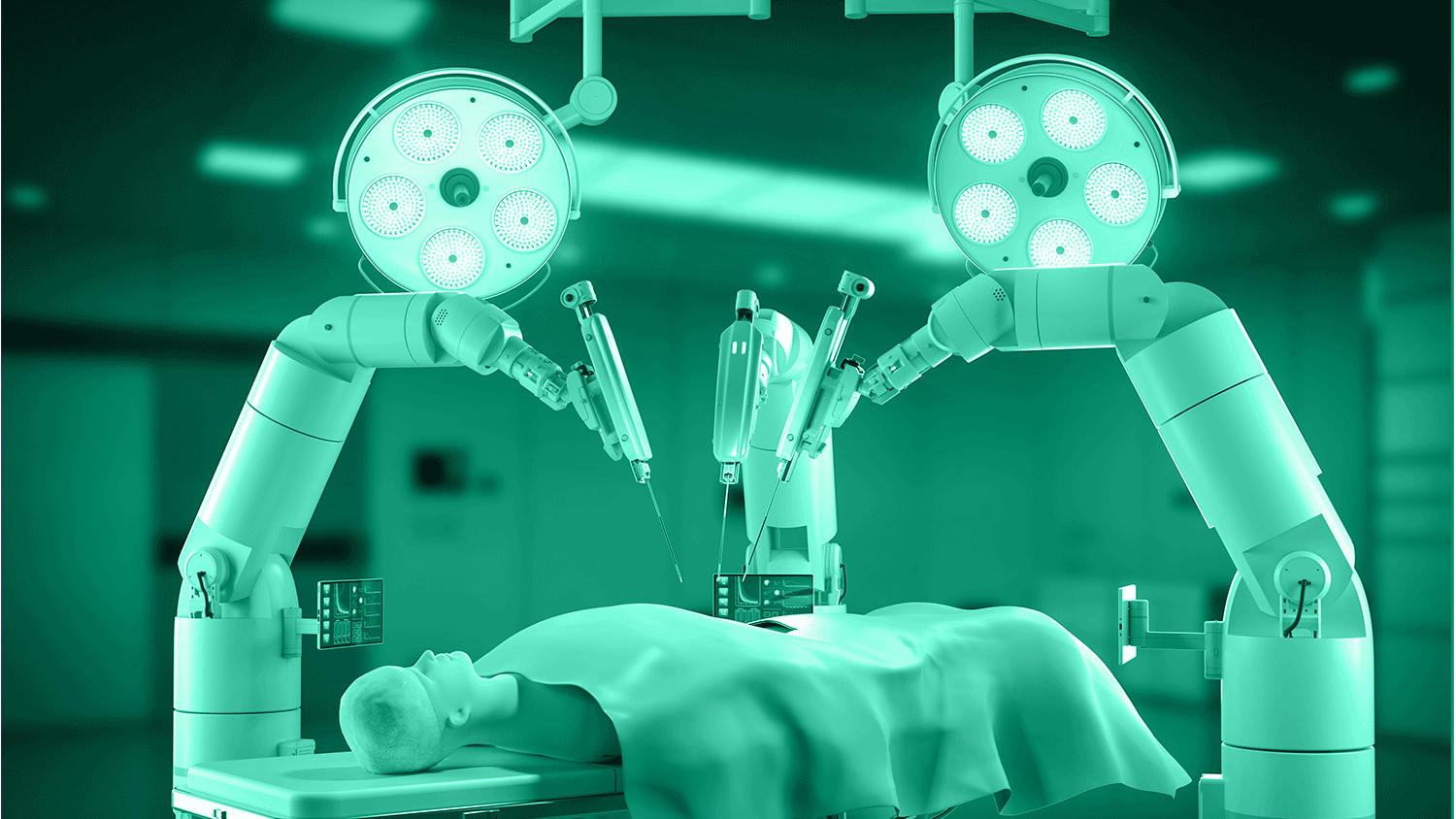
Modern treatments are those treatments which use advanced Medical technologies which can cure the disease in lesser time with less pain and with more accuracy.
Insurers have identified below ailments as modern treatments.
- Uterine Artery Embolization and HIFU
- Balloon Sinuplasty
- Deep Brain stimulation
- Oral chemotherapy
- Immunotherapy- Monoclonal Antibody to be given as an injection
- Intravitreal injections
- Robotic surgery
- Stereotactic radiosurgery
- Bronchial Thermoplasty
- Vaporisation of the prostate (Green laser treatment or holmium laser treatment)
- IONM – (Intra Operative Neuro Monitoring)
- Stem cell therapy: Hematopoietic stem cells for bone marrow transplant for hematological conditions to be covered.
What about our Clients' claim?
Eventually the Insurer had to pay the whole amount.
Today all insurers are mandated to cover modern treatments by the Regulator. Most insurers have very low sub-limits on these treatments, just so that they can meet the IRDAI guidelines.
How many of you have gotten the Modern Treatments covered without any sub-limits in your Group Mediclaim Policy?